Exercise Modalities for Chronic Respiratory Disease Management
Chronic respiratory diseases, such as asthma and chronic obstructive pulmonary disease (COPD), profoundly affect individuals’ quality of life. Incorporating specialized exercise modalities can significantly enhance management strategies for these conditions. Exercise improves respiratory function, reduces dyspnea, and increases overall physical endurance. Engaging in physical activity also promotes mental well-being and social interaction, which are vital for symptomatic relief. Effective exercise programs are tailored to the individual’s specific health concerns and physical capabilities. These programs often include elements such as aerobic training, strength training, and stretching exercises. Aerobic training particularly benefits patients by improving lung capacity and oxygen utilization. Strength training enhances muscle function, vital for daily activities, making it easier to perform tasks. Additionally, practicing flexibility through stretching minimizes the risk of injuries and enhances mobility. Individuals with chronic respiratory diseases should consult healthcare professionals before starting any exercise regimen, ensuring that their specific needs are accurately addressed. Overall, with the proper framework and professional guidance, exercise can become an integral part of the chronic respiratory disease management plan.
The choice of exercise modalities is crucial for individuals managing chronic respiratory diseases. Each form of exercise serves a distinct purpose and delivers specific benefits. For example, low-impact aerobics can significantly improve cardiovascular endurance while minimizing joint stress. Specific activities like swimming or cycling may benefit patients with respiratory difficulties, as they provide resistance and support breathing. Similarly, resistance training helps in improving muscle strength and functional capacity while ensuring a manageable intensity level. Furthermore, balance exercises can minimize the risk of falls and enhance body control, enabling patients to engage better in daily scenarios. Patients often find motivation through group exercise classes, where they can participate in supportive environments with others facing similar challenges. Various community programs are available that focus solely on chronic disease management through exercise, further promoting adherence to physical activity. Importantly, patients must set realistic and achievable goals to track progress over time. Tracking improvements boosts motivation and provides insights into the effectiveness of their exercise routines. Therefore, exploring diverse modalities enables patients to find what resonates most with them in achieving optimal health outcomes.
In addition to structured exercise, incorporating daily physical activity is vital for those managing chronic respiratory diseases. Patients can engage in simple activities such as walking, gardening, or even household chores to maintain regular movement. Such activities not only contribute to physical fitness but also support pulmonary health by encouraging optimum lung function and capacity. Patients should gradually increase activity levels according to their capabilities and responsiveness to exercise recommendations. For some, the introduction of wearable fitness trackers can aid significantly in ensuring that daily objectives are met. Evaluating physical performance through such devices can motivate individuals to remain active and committed to their health goals. Furthermore, understanding the significance of pacing is essential. Patients must learn to listen to their bodies and adjust activity intensity and duration according to their needs. Complementing these efforts with breathing techniques and relaxation exercises can further enhance respiratory function. Techniques like diaphragmatic breathing can improve ventilation and oxygenation levels. Thus, daily activity alongside planned exercise constitutes a comprehensive approach to managing chronic conditions effectively, fostering a balanced lifestyle that prioritizes health and well-being.
Challenges in Exercise Implementation
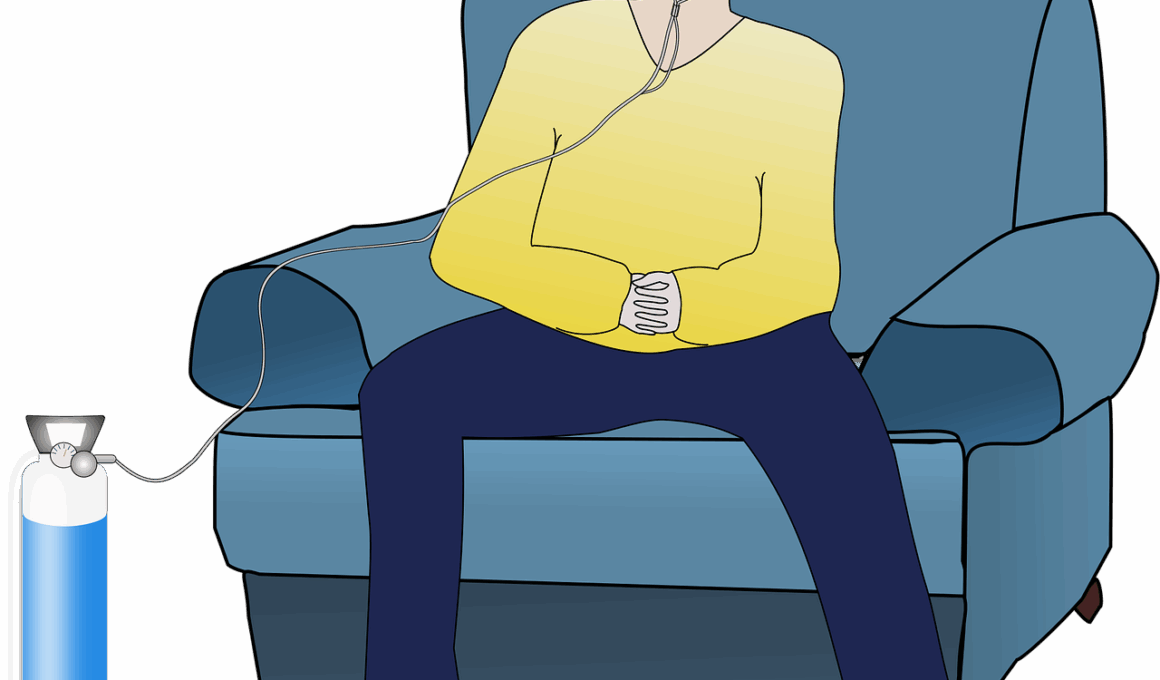
Despite the numerous benefits of exercise, patients with chronic respiratory diseases may face significant barriers to participation. Common challenges include shortness of breath, fatigue, and limitations in physical endurance. These factors often discourage individuals from engaging in consistent physical activity, resulting in reliance on medication without concurrent lifestyle changes. Additionally, fear of exercise-related exacerbations may lead to avoidance behavior. It is crucial for healthcare providers to address these concerns and validate patients’ experiences, helping them to build confidence in their ability to exercise safely. Customized exercise programs and ongoing support from practitioners can alleviate fears by guiding individuals in managing their symptoms effectively. Education about warning signs and the importance of pacing during activity can further empower patients. Moreover, promoting a supportive environment helps foster relationships among patients with similar experiences. Emotional support from peers undergoing similar challenges plays a significant role in encouraging participation. By confronting these barriers head-on with actionable strategies, healthcare professionals can facilitate greater involvement in physical activity that enriches patients’ lives and overall health outcomes.
Engaging with exercise specialists or physical therapists familiar with chronic respiratory conditions enhances program effectiveness. These professionals help design individualized exercise plans that align with specific health profiles and limitations. Supervised exercise training offers structured environments, promoting safety and efficiency. These programs provide essential education on how to exercise safely, recognize and manage symptoms, and set achievable goals based on individual performance levels. Moreover, ongoing assessments enable personalized adjustments to the exercise plan as fitness levels improve. By incorporating components such as endurance, strength, and flexibility training, specialists can create comprehensive strategies that address all facets of physical fitness. Patients may also access educational workshops that build their knowledge of exercise physiology and disease management. Understanding the physiological basis for why exercise benefits respiratory health empowers individuals and fosters engagement in their exercise regimes. Consequently, patients are more inclined to take responsibility for their health and well-being, leading to more successful outcomes. This approach illustrates the importance of integrating expert guidance, educational resources, and supportive communities in fostering an active lifestyle for those with chronic respiratory illnesses.
Importance of Nutrition Alongside Exercise
Exercise is vital but becomes even more effective when combined with proper nutrition. Nutritional status plays a significant role in managing chronic respiratory diseases, as deficiencies can worsen disease progression. An appropriate diet helps maintain optimal body weight, supports immune function, and enhances recovery. Many healthcare providers emphasize the importance of a balanced diet rich in essential nutrients, particularly antioxidants, which support lung health. Foods such as fruits, vegetables, nuts, and fish contribute significantly to nutritional intake. Clinicians often recommend the Mediterranean diet, which focuses on heart-healthy components and minimizes processed foods. Additionally, adequate hydration is fundamental to maintaining effective mucus clearance within the respiratory passages. Patients should aim to drink plenty of fluids to promote optimal respiratory function. Supplementing with anti-inflammatory nutrients can also support overall lung health. Consulting with a registered dietitian who specializes in chronic disease can greatly enhance individual dietary plans. This collaboration ensures patients gain access to personalized advice that factors in food preferences, cultural values, and nutritional needs. Thus, parallel attention to nutrition complements exercise regimes, optimizing management strategies for chronic respiratory diseases.
Finally, the execution of exercise for respiratory disease management should focus on long-term adherence and lifestyle changes. Training adherence is significantly influenced by establishing routines and setting personal motivations. Those who view exercise as an essential aspect of their health are more likely to sustain ongoing participation. The support of family, friends, and healthcare teams enhances commitment levels as well. Regular follow-up appointments with healthcare providers can reinforce the significance of physical activity and its advantages. Additionally, wellness programs fostering community engagement equip individuals with the camaraderie needed to persist in their exercise commitments. Social connections not only enhance emotional well-being but also nurture accountability within exercise routines. Moreover, celebrating milestones, such as improved endurance or strength gains, increases patient confidence and motivates continued efforts. Utilizing goal-setting tips and strategies promotes progress and instills a sense of achievement. By adopting a comprehensive approach toward routine physical activity and support systems, individuals gain the necessary tools to combat chronic respiratory diseases effectively, leading them toward valuable improvement in their health and quality of life.