The Impact of Diabetic Neuropathy on Quality of Life and How to Cope
Diabetic neuropathy is a common complication of diabetes, affecting the peripheral nerves and causing various symptoms that impact individuals’ lives significantly. This condition can lead to painful sensations, numbness, and weakness in the limbs, ultimately diminishing the quality of life. Many individuals suffering from diabetic neuropathy experience a decline in emotional well-being due to chronic pain and discomfort. They may also find limitations in mobility that interfere with daily activities, making even mundane tasks challenging. The impact of this condition is not only physical but also psychological. Studies have shown that neuropathy can contribute to feelings of anxiety and depression, further complicating diabetes management efforts. Effective coping strategies for those affected are essential to improving their quality of life. Medical interventions such as medication for pain relief and lifestyle modifications including diet and exercise can be beneficial. Support from healthcare professionals can provide guidance in managing the symptoms. Furthermore, engaging in support groups can help individuals feel less isolated, allowing them to share experiences and coping strategies with others who understand their struggles. This holistic approach can empower patients to actively manage their health.
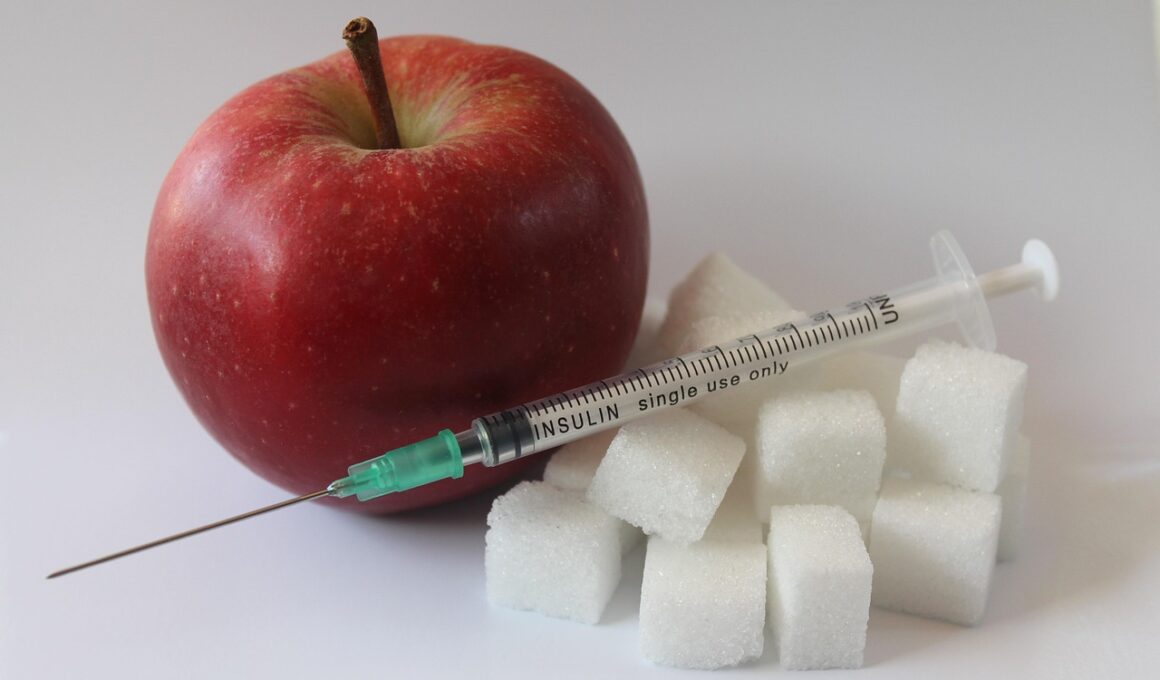
Maintaining optimal blood sugar levels is crucial in managing diabetic neuropathy effectively. Poor glucose control can exacerbate nerve damage, leading to worsened symptoms and increased discomfort. By focusing on proper diabetes management through regular monitoring of blood sugar levels, patients can effectively mitigate the progression of neuropathy. Implementing dietary changes is one effective way to achieve better glucose control. A balanced diet rich in whole foods, such as vegetables, lean proteins, and healthy fats, promotes stable blood sugar levels. Moreover, limiting refined sugars and processed carbohydrates can prevent sudden spikes in glucose. Physical activity is also essential in managing diabetes and neuropathy. Engaging in regular exercise can improve circulation, reduce stress, and promote overall health. Even low-impact activities like walking, swimming, or cycling can be beneficial. Patients should consult with their healthcare providers to create a tailored exercise plan that abides by their fitness levels and capabilities. Additionally, incorporating resistance training can enhance muscle strength and support nerve function. Staying hydrated and managing weight can be further helpful in maintaining overall health and mitigating symptoms. These strategies can foster a sense of control over health challenges.
Coping Mechanisms for Pain Management
Pain management is a key aspect of coping with diabetic neuropathy. Chronic pain can be debilitating and create a significant burden in various areas of life, including work and social interactions. Effective pain relief strategies are therefore essential to improve quality of life. Incorporating both pharmacological and non-pharmacological approaches can result in better overall management. Medications, such as anticonvulsants and antidepressants, are often prescribed to help alleviate neuropathic pain. Adjusting dosages and treatment plans based on individual needs is crucial, thus open communication with healthcare providers is encouraged. Additionally, employing complementary therapies can provide further relief; practices such as acupuncture, physical therapy, and transcutaneous electrical nerve stimulation (TENS) have been reported to help many patients. Mindfulness techniques, including meditation and deep-breathing exercises, can also reduce pain perception and offer relaxation. Patients should actively explore various modalities for pain relief while remaining closely connected with their healthcare team. This tailored approach allows individuals to discover which methods work best for them personally, leading to a more satisfying life experience despite living with diabetic neuropathy. Education on self-management techniques can empower patients greatly.
In addition to pain management, addressing the emotional and psychological aspects of diabetic neuropathy is vital. Many individuals with this condition find themselves dealing with frustration, sadness, and feelings of helplessness as they navigate the challenges of their symptoms. Seeking emotional support from friends, family, or mental health professionals can significantly mitigate these feelings. Participating in therapy can provide individuals with coping strategies and tools to manage their emotional responses. This allows them to focus on their strengths rather than limitations, facilitating a more positive outlook. Support groups specifically tailored for those with chronic pain conditions can foster camaraderie and connection, allowing participants to share their successes and challenges openly. Educating oneself about diabetic neuropathy can also alleviate anxiety surrounding the unknown, offering hope as patients learn what to expect and how to cope effectively. Journaling can serve as another form of self-expression, allowing individuals to process their thoughts and feelings in a private setting. Combining emotional and psychological support with physical care creates a well-rounded approach to managing diabetic neuropathy, enhancing the overall quality of life for patients.
The Importance of Regular Check-Ups
Regular check-ups with healthcare professionals play a pivotal role in the management of diabetic neuropathy. Monitoring the condition closely allows for timely interventions that can prevent further progression of nerve damage. Comprehensive evaluations may involve routine blood tests, assessments of nerve function, and foot examinations to identify any potential complications early. This proactive approach can identify problems before they escalate, ensuring prompt treatment options are available. Attending diabetes management classes can also be beneficial, providing patients with up-to-date information on healthcare practices and lifestyle modifications. These classes often focus on managing diabetes comprehensively, including dietary recommendations, exercise tips, and medication management. Furthermore, engaging in patient-provider communication during these visits ensures that concerns and symptoms are addressed, leading to better personalized care. Ensuring open lines of communication fosters trust and encourages patients to be proactive in discussing any new symptoms or difficulties they’re experiencing. By committing to regular follow-ups, patients make significant strides in their health journey, equipping themselves with knowledge and strategies to cope effectively with diabetic neuropathy.
Adaptation to a new lifestyle is often necessary for individuals experiencing the effects of diabetic neuropathy. Acknowledging the challenges posed by this condition is an important step in making the required adjustments. Establishing a routine can help individuals adapt to their new normal while ensuring consistent attention to health and wellness. It can be beneficial for patients to create daily schedules that incorporate time for exercise, healthy meal preparation, medication management, and relaxation techniques. Setting realistic, achievable goals can help in fostering a sense of accomplishment and purpose in daily life. Additionally, technology can support diabetes management, with various apps available for tracking blood sugar, meals, and physical activity. Many diabetes-specific devices also help monitor health conditions more intuitively, providing valuable data for patients and healthcare providers alike. Sharing successful strategies and progress within a support network can further maintain motivation and accountability while providing the emotional validation that is often necessary. Adapting effectively involves cultivating resilience and developing a robust support system that ultimately empowers individuals to confront the challenges of diabetic neuropathy with greater strength.
Seeking Professional Help
While self-management strategies play an integral role in dealing with diabetic neuropathy, seeking professional help remains imperative for long-term success. Healthcare providers are critical allies in guiding treatment plans, ensuring patients receive appropriate care to address their needs continually. They can also connect patients with specialists, such as neurologists or dietitians, who can provide focused interventions tailored to individual circumstances. Open dialogue about symptoms and challenges facilitates the identification of additional support resources, such as occupational therapy or pain management clinics, that can greatly enhance the patient experience. For some individuals, exploring the possibility of clinical trials related to diabetic neuropathy may reveal new options for treatment not yet widely available. Information about ongoing studies can help pave the way for innovative therapies that can improve their quality of life significantly. Patients should not hesitate to reach out to their healthcare teams, discussing any changes as they arise. Regular check-ins and adjustments in care are vital to maintain optimal health and impede the progression of diabetic neuropathy. By remaining engaged in their healthcare journey, patients can take control, ensuring they receive the support they need in their fight against this challenging condition.
In conclusion, dealing with diabetic neuropathy requires a multifaceted approach that encompasses physical, emotional, and psychological care. Each aspect of this condition is interconnected; therefore, neglecting one element can hinder overall progress. Adopting proactive strategies such as regular blood sugar monitoring, dietary changes, and physical activity can significantly impact symptom management and overall well-being. Emotional support from families, friends, therapists, or support groups can help enhance resilience and coping strategies. Utilizing technology, staying informed, and establishing effective routines can empower patients to navigate their challenges regularly and purposefully. Regular health check-ups and open communication with healthcare professionals remain critical in managing neuropathy successfully. By acknowledging the complexities of diabetic neuropathy and seeking appropriate help and resources, individuals can create a pathway toward a better quality of life. Ultimately, the journey may involve trials and challenges, but with determination and the right support, individuals can adapt and thrive. Education, self-advocacy, and community support play crucial roles in building resilience and dealing effectively with this chronic condition. This comprehensive approach ultimately leads to improved health outcomes and a richer quality of life for those affected by diabetic neuropathy.