Flexibility and Mobility Assessment in Rehabilitation Settings
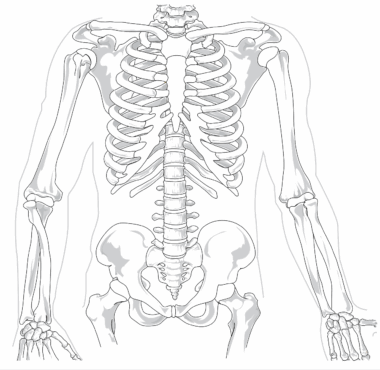
Flexibility and mobility assessments are essential components in rehabilitation settings. They help determine the range of motion, strength, and endurance of patients recovering from injuries. Assessing flexibility involves examining the ability of muscles and joints to move freely, which is crucial for everyday activities. Healthcare professionals often utilize various techniques, including goniometry and functional movement screenings, to evaluate patients’ conditions accurately. Goniometry specifically measures angles at joints, providing quantitative data on an individual’s flexibility. Additionally, assessments can identify specific limitations or imbalances within the body that may hinder rehabilitation efforts. In conjunction with mobility assessments, flexibility evaluations aim to understand how a patient’s overall functionality can improve throughout therapy. This comprehensive approach allows for tailored intervention plans that address individual needs effectively. Regular assessments also help track progress, making it easier for therapists to adjust treatment protocols as necessary. Utilizing flexibility and mobility assessments in rehabilitation ensures a holistic view of a patient’s capabilities, laying the groundwork for successful recovery and improved life quality. The ultimate goal is to help patients regain full functionality and independence in their daily activities while minimizing the risk of re-injury.
The importance of flexibility cannot be overstated in rehabilitation settings. Through assessments, therapists can identify muscle tightness or joint stiffness that could affect mobility. This evaluation process typically includes dynamic and static stretching exercises to ascertain core flexibility levels. Moreover, balance assessments are also critical as they correlate directly with effective mobility. When flexibility limitations are identified, targeted stretching programs can be initiated to enhance range of motion. These programs often incorporate specific exercises designed to strengthen muscles while promoting greater flexibility. Furthermore, the relationship between flexibility and age, gender, and overall physical condition is examined through these assessments. This understanding allows therapists to personalize treatment plans based on individual patient profiles. Additionally, educational resources can guide patients on maintaining their flexibility through daily practices. In essence, mobility and flexibility assessments serve to empower patients, engaging them actively in their rehabilitation journey. By understanding their physical limitations, patients often feel more motivated to participate in recommended therapies. Ultimately, assessments serve as an essential first step toward achieving optimal recovery and enhancing life quality, paving the path for patients to reclaim their active lifestyles.
Techniques for Assessment
Various techniques are utilized in flexibility and mobility assessments within rehabilitation settings. One such method includes passive and active assessments, which examine flexibility through the examiner’s assistance or the patient’s movements. Another popular technique involves the Sit and Reach Test, which primarily focuses on hamstring and lower back flexibility. This test can highlight underlying issues and help design suitable exercise regimens. In addition to this, the Thomas Test is useful for evaluating hip flexor tightness. It measures the ability of the hips to move freely and is particularly valuable for athletes or active individuals. These assessments provide insights into how well patients can perform everyday activities without discomfort. Moreover, the Functional Movement Screen (FMS) has gained prominence as a means to assess mobility patterns through a series of movements. FMS identifies compensatory movements that can lead to injuries over time. Incorporating multiple techniques offers a comprehensive profile of a patient’s capabilities, ultimately guiding treatment options effectively. It is vital for therapists to remain attentive to assessment outcomes, using the data to adjust therapeutic interventions according to progress noted during rehabilitation.
Individualized treatment programs stem from these assessments, ensuring that each patient’s unique needs are addressed. Based on flexibility and mobility evaluations, rehab specialists can outline exercise plans promoting optimal recovery. These plans often incorporate stretching routines, strengthening activities, and balance exercises. For instance, static stretching can be prescribed to improve overall flexibility while dynamic stretching can effectively prepare the body for physical activity. Essential elements of mobility training include gait and balance exercises designed to enhance overall stability and coordination. Furthermore, the integration of modalities like foam rolling and physical therapy can complement flexibility training. Foam rolling can assist in alleviating muscle tightness, leading to improved range of motion. Additionally, educating patients on the significance of maintaining flexibility and mobility helps them understand their pivotal role in recovery. As patients engage actively in their treatment, success rates tend to rise. Overall, individualized approaches rooted in thorough assessments pave the way for effective rehabilitation. Regular follow-ups allow for modifications in exercise routines, ensuring continuous improvement in flexibility and mobility. The goal remains to restore confidence in movements, enabling patients to participate fully in their daily lives.
Challenges in Flexibility Assessment
Flexibility and mobility assessments present unique challenges within rehabilitation settings. One primary issue revolves around standardization, as different therapists may use diverse techniques and tools. This lack of uniformity can result in inconsistent evaluation outcomes, jeopardizing treatment effectiveness. Additionally, understanding patient limitations due to pain or discomfort may hinder accurate assessments. Pain often influences an individual’s willingness to engage fully in evaluation activities. It is essential for therapists to create a supportive atmosphere where patients feel comfortable expressing discomfort. Another challenge involves the varying adaptability to different assessment tools. Not all patients may be familiar with techniques like goniometry or the sit-and-reach test, impacting the accuracy of results. Moreover, certain cultural factors may affect patient perceptions of mobility and flexibility, which can inadvertently influence assessment outcomes. Consequently, it is vital for therapists to be sensitive to individual backgrounds during assessments. Addressing these challenges requires continual professional development and education for healthcare providers. By fostering an environment that acknowledges complexity in flexibility assessments, therapists can better facilitate patient recovery and improve rehabilitation protocols. Ultimately, these efforts enable therapists to deliver comprehensive care aimed at optimizing patient outcomes.
Monitoring progress from flexibility and mobility assessments holds significant value in rehabilitation. Regular assessments allow therapists to evaluate the effectiveness of implemented strategies, aligning treatment with each patient’s evolving needs. By documenting changes over time, practitioners can garner valuable insights into what interventions yield the best outcomes. Patients benefit tremendously from understanding their progress, which fosters motivation and commitment to treatment. Furthermore, assessment data can guide therapists in adjusting or intensifying exercises as needed. One effective strategy includes the use of visual feedback, helping patients grasp their improvement visually. For example, demonstrating an increase in range of motion via comparison initially measured can enhance patient understanding. Additionally, considering peer support helps patients share experiences and challenges faced during recovery. This encouragement reinforces their recovery journey while validating individual efforts. Moreover, collaborative assessments involving interdisciplinary teams can enhance the therapeutic experience, allowing for holistic feedback. Ultimately, monitoring progress through regular assessments is crucial for refining treatment goals, ensuring patients continually work towards improved flexibility and mobility. This positive reinforcement sustains high levels of engagement, promoting not only physical healing but overall well-being.
Conclusion and Future Directions
As flexibility and mobility assessments evolve, the future of rehabilitation looks promising. Technological advancements are paving the way for more sophisticated assessments, enhancing accuracy and patient engagement. Wearable devices and mobile applications can provide continuous monitoring of flexibility and mobility, offering real-time feedback. This data can lead to more personalized treatment plans, maximizing patient outcomes. Furthermore, conducting research on the correlation between flexibility levels and specific health issues can strengthen the integration of mobility assessments into rehabilitation. Such insights contribute to evidence-based approaches in healthcare settings. Additionally, further interdisciplinary collaboration can enhance assessment methods, enabling diverse perspectives to shape treatment protocols. The growing emphasis on preventive care also underscores the importance of flexibility and mobility assessments in prolonging health. Educating patients on the role of flexibility in injury prevention can empower them to take charge of their physical health. Overall, embracing innovation while maintaining core assessment techniques ensures a comprehensive approach to rehabilitation. Future directions in flexibility and mobility assessments will likely prioritize patient-centered care and ongoing education as fundamental elements. Consequently, improved methods will elevate therapy standards and significantly enhance recovery experiences.
In summary, flexibility and mobility assessments form an integral aspect of rehabilitation settings. By employing various evaluation techniques, therapists gain essential insights into patient limitations and strengths. These insights directly inform treatment plans, enabling personalized care that optimally supports recovery. Moreover, the challenges inherent in conducting flexibility assessments highlight the need for continual innovation and refinement in techniques. Emphasizing patient education and progress monitoring ensures effective rehabilitation outcomes, as individuals become more engaged in their recovery journey. Preparing for future advancements also sets the stage for transformative changes in rehabilitation practices. The integration of technology and interdisciplinary approaches will likely enhance assessment accuracy while enabling timely interventions. Flexibility and mobility assessments serve as the foundational tools for therapists, guiding patient recovery towards improved quality of life. Therefore, prioritizing research and development in these areas remains crucial. Ultimately, a patient-centered approach that embraces ongoing assessment will yield significant benefits, promoting not just physical recovery but greater autonomy in day-to-day life. Such practices exemplify the evolving landscape of rehabilitation, where flexibility and mobility are recognized as essential components of comprehensive patient care.