Augmented Reality Tools for Diabetes Education and Training
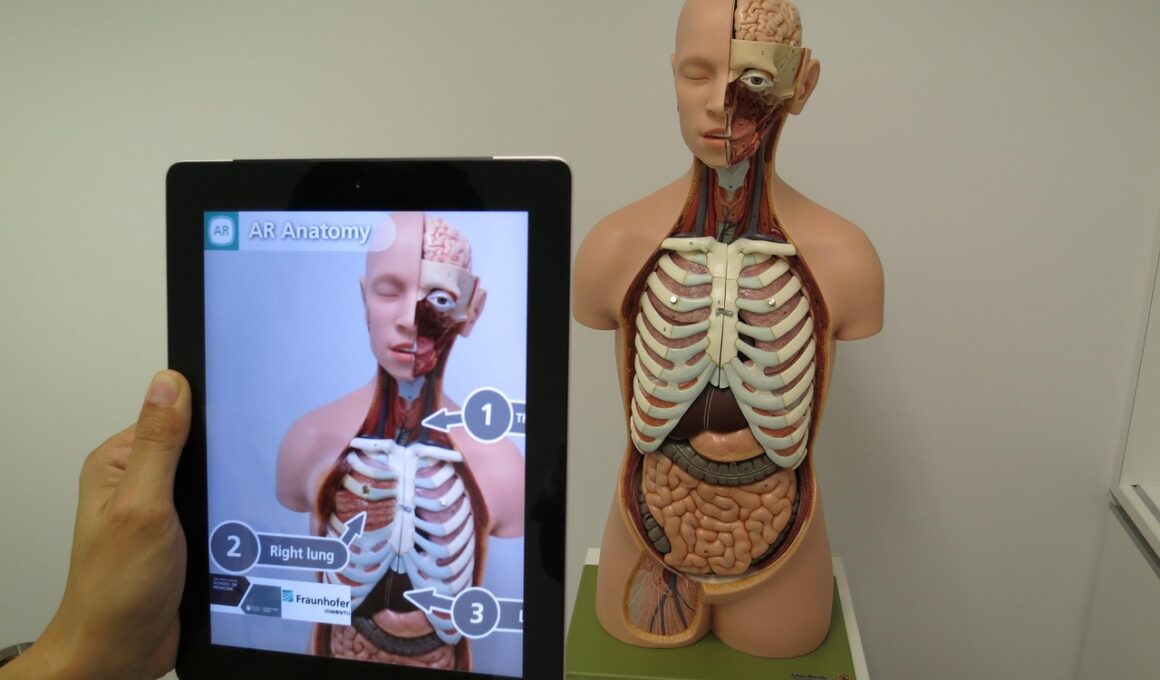
Diabetes management has progressed greatly with advances in technology, specifically augmented reality (AR) tools designed for education and training. These tools enhance the learning experience for patients, caregivers, and healthcare professionals by creating immersive environments. AR allows real-time interaction with the digital information layered over the physical world, providing insights that can demystify the complexity of diabetes care. For example, AR applications can visualize the effects of carbohydrate intake on blood sugar levels, helping patients understand the impact of their dietary choices. This interactive technology can also simulate insulin administration techniques, making it easier for users to grasp essential skills without the typical stress and uncertainty associated with traditional methods. Moreover, healthcare providers can use AR for more effective training and assessment, ensuring that patients master the fundamental aspects of diabetes self-management. By engaging patients in a dynamic, stimulating manner, AR tools help not only inform users but also motivate them to adhere to their treatment plans. The integration of AR into diabetes education offers unprecedented opportunities for personalized care and improved outcomes.
Benefits of Augmented Reality in Diabetes Education
The benefits of using augmented reality tools in diabetes education are numerous and impactful. These tools provide a more engaging learning experience, which is crucial for patients who often face overwhelming amounts of information. By employing 3D visualizations and interactive content, AR can help simplify complex processes like insulin injection and glucose monitoring. Enhanced retention of knowledge is another significant advantage, as users can visualize and manipulate information in real-time. Practicing techniques in a simulated environment prepares patients for real-life situations, boosting their confidence and reducing anxiety associated with diabetes care. Additionally, AR tools can be customized to meet the unique needs of each patient, offering personalized training that aligns with individual lifestyle choices. This adaptability is essential in a disease as varied as diabetes, where one size does not fit all. Having instant access to information through AR applications also enables patients to make informed decisions quickly. Overall, integrating AR in diabetes education leads to improved health outcomes by promoting effective self-management and informed decision-making.
Healthcare professionals also benefit significantly from AR tools designed for diabetes management training. These applications can provide advanced resources for understanding diabetes pathophysiology and the nuances of treatment algorithms. By enhancing medical training with AR, professionals can visualize patient cases and scenarios through simulations that mimic real-life challenges. This interactive approach encourages better diagnostic skills and improves communication with patients. Additionally, healthcare providers gain insights into potential complications, allowing them to prepare their patients adequately for the challenges ahead. The ability to visualize glucose metabolism and the effects of different treatments within a 3D environment lends itself to a deeper understanding of patient care strategies. Moreover, AR can assist in continuing education for professionals, enabling them to stay current with medical advancements in diabetes care. Collaborating through AR with peers or mentors leads to enhanced skill-sharing and collective problem-solving. This synergy among healthcare professionals ultimately benefits the patient population, resulting in higher standards of diabetes care and improved patient outcomes through innovative training methodologies.
Challenges of Implementing Augmented Reality
Despite its numerous advantages, implementing augmented reality tools in diabetes education is not without challenges. The high costs associated with developing and implementing these technologies can be prohibitively expensive for healthcare systems. Additionally, there is a need for sufficient technological infrastructure and support to facilitate AR’s effective use, particularly in rural or underserved areas. Staff training is equally vital, as healthcare providers must be comfortable using AR tools to extract the full potential of these resources. Furthermore, there is often a resistance to change within traditional healthcare settings, making it difficult to introduce new methods. Patients may also face hurdles, such as lack of access to smartphones or tablets that support AR-applications. User interface design plays a crucial role in ensuring that these applications are user-friendly and can cater to those with varying levels of technological comfort. Lastly, the potential for information overload exists; thus, the design must effectively communicate essential information without overwhelming users to avoid confusion during learning. Addressing these challenges is essential for the successful integration of AR tools into diabetes education.
Future developments in augmented reality tools for diabetes management hold great promise. Emerging innovations aim to address current challenges, enhancing the delivery of education and training programs for patients and healthcare providers alike. As AR technology advances, collaboration with software developers and healthcare professionals will be crucial in creating tailored applications that serve diverse user needs. The incorporation of artificial intelligence into AR tools is an exciting avenue, providing personalized user experiences and feedback based on individual user behaviors and preferences. Continuous evolution of these tools will allow for seamless integration into various aspects of diabetes care, enabling real-time adaptations and updates. Additionally, increased accessibility to mobile devices will foster wider acceptance and use cases for AR applications, ensuring that more patients can benefit from innovative educational resources. Future research should focus on the effectiveness of AR in raising diabetes awareness and improving health literacy among diverse populations. By developing a robust evidence base showcasing the efficacy of AR tools, stakeholders can foster confidence and support in their broader application in diabetes management.
Real-World Applications of AR in Diabetes Care
Several successful real-world applications have emerged that illustrate the effectiveness of augmented reality tools in diabetes care. For instance, educational programs are incorporating AR experiences to guide patients through the complex management of their condition, which improves both understanding and engagement. One such program allows users to practice injection techniques in a simulated environment, reducing anxiety and increasing confidence in handling their diabetes management. Other initiatives have utilized AR for community health events, allowing individuals to visualize their health data interactively, fostering awareness concerning blood glucose levels and lifestyle choices. Moreover, AR has been employed in developing comprehensive training programs for healthcare providers, enhancing their ability to communicate effectively with patients. Research studies have demonstrated that those trained through AR utilize techniques more proficiently in clinical settings, leading to better patient outcomes. Healthcare institutions that invest in AR technology report increased patient satisfaction due to improved educational clarity and comprehension. As these success stories spread, more organizations are likely to explore integrating AR tools into existing training frameworks, paving the way for enhanced diabetes education and ultimately better health management.
Overall, integrating augmented reality tools into diabetes education and training presents a transformative opportunity for both patients and healthcare professionals. As technology continues to evolve, the benefits of AR in enhancing learning processes, providing effective training, and improving patient outcomes will become increasingly evident. The potential for personalized education experiences tailored to individual learning styles is particularly promising, as this adaptability mirrors the unique needs of each diabetes patient. Future research should continue to focus on overcoming the barriers associated with implementing these advanced tools while highlighting their effectiveness in real-world scenarios. As the healthcare landscape adapts to incorporate innovative solutions, the emphasis on education will remain pivotal in empowering individuals to manage their diabetes effectively. Harnessing the strengths of augmented reality can lead to a more informed patient population, ultimately fostering better disease management and healthier lives. Embracing these technologies marks a vital step toward a future where diabetes education is engaging, interactive, and effective, ensuring that patients receive the knowledge and skills necessary to thrive.