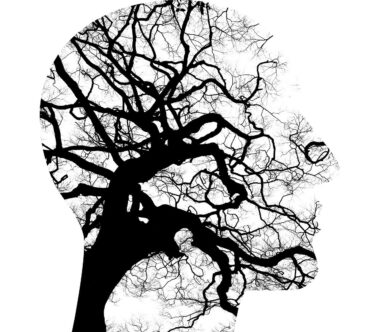
Common Myths and Facts About Obsessive-Compulsive Disorder
Obsessive-Compulsive Disorder (OCD) is often misunderstood. Many believe it’s a personality quirk rather than a mental health condition. People often confuse OCD with being overly neat or organized, but it actually involves distressing obsessions and compulsions. Obsessions are intrusive thoughts that cause anxiety, while compulsions are behaviors performed to reduce that anxiety. It’s crucial for society to recognize that OCD affects individuals across diverse backgrounds and can severely impact daily functioning. This common misconception can lead to stigma, which further deters people from seeking help. Many individuals with OCD experience a range of symptoms that differ significantly from one person to another, demonstrating the disorder’s complexity. Treatment is available, making early intervention essential. Misunderstanding OCD perpetuates misinformation and can prevent those suffering from receiving the necessary support and resources. Awareness can save lives and significantly enhance the quality of life for individuals with OCD. Thus, it is vital for information to circulate and educate the public about this prevalent yet significantly misunderstood condition. With increased understanding comes compassion, helping to uplift those affected by OCD. Being informed is the first step towards fostering a supportive community.
Myth 1: People with OCD are just perfectionists. This stereotype reduces OCD to a glorified version of being tidy. In reality, many individuals with OCD experience violent thoughts or irrational fears that drive their compulsive behaviors. Describing OCD solely through the lens of perfectionism disregards the severity and pain of the condition. It’s an emotional burden that extends far beyond a desire for order. People with OCD may carry out rituals, like washing their hands excessively or checking locks multiple times, as a desperate attempt to alleviate anxiety. This overlooks how debilitating OCD can be; the disorder often leads to excessive time spent on rituals, which can interfere with daily activities. It’s essential to understand that the display of compulsions is an effort to combat overwhelming anxiety rather than an inclination towards perfectionism. Acknowledging this difference can foster empathy and understanding. Treatment options, such as cognitive behavioral therapy and medication, help those affected regain control over their lives. Education about OCD’s true nature facilitates compassion, supportive dialogue, and invites the possibility of recovery. By dismantling myths, we can create an environment where people feel safe discussing their experiences with OCD.
The Reality of OCD
Fact: OCD is an anxiety disorder that affects millions worldwide. It’s estimated that about 1 in 40 adults and 1 in 100 children suffer from this condition. As pervasive as it is, many still regard OCD as a personal failing or a joke, a misconception that minimizes its impact. Many people face extreme distress due to unwanted thoughts, leading to irrational fears. For example, someone with OCD might worry excessively about contamination, driving them to compulsively wash their hands or avoid certain environments altogether. This behavior is not a choice; it’s a part of the mental struggle they experience daily. Emotional challenges can cause severe isolation and may lead to secondary conditions, such as depression. Recognizing OCD as a legitimate mental disorder means that those experiencing it deserve compassion and access to treatment. Effective therapies, such as exposure and response prevention (ERP), are available for individuals facing this struggle. By understanding these facts about OCD, we can help shift the narrative and provide support for individuals seeking recovery. A more informed society can take actionable steps to help advocate for better resources and treatment options for those affected.
Myth 2: OCD is just about cleanliness and order. While some individuals associate OCD with being tidy, this portrayal is misleading and overly simplistic. People with OCD may experience a variety of obsessions and compulsions, not solely related to cleanliness. Some may obsess about safety, leading to compulsive checking behaviors, such as repeatedly checking if doors are locked or if the stove is off, even when they know it is. This illustrates how OCD encompasses many aspects of an individual’s life. These rituals often consume hours, ruling their daily activities and draining their energy and time. The focus on cleanliness overshadows the broader range of symptoms. For instance, individuals might experience intrusive thoughts about harming themselves or others, which can lead to severe anxiety. Education around OCD must highlight the diverse nature of this disorder to encourage individuals to seek help without feeling judged. Acknowledging the spectrum of OCD allows for understanding and acceptance. Debunking this myth empowers people to come forward, enabling a more open dialogue about their experiences and fostering an environment in which they feel safe to discuss their challenges.
Understanding OCD Symptoms
Fact: Symptoms of OCD vary widely among individuals. While some may experience significant compulsive behaviors, others may primarily deal with distressing thoughts without engaging in visible rituals. This variety showcases how unpredictable OCD can be. The disorder’s hallmark is the presence of obsessions—unwanted, intrusive thoughts that provoke anxiety. These can include exaggerated fears about contamination, loss of control, or harming others. To cope with this anxiety, individuals may result in responding behaviorally, performing compulsions that alleviate those upsetting feelings temporarily. Unfortunately, these compulsions don’t resolve the underlying anxiety, leading to a cycle of compulsions and obsessions. This differentiates OCD from other mental health disorders, ensuring that understanding varies across the spectrum of experiences. Therefore, it is vital for healthcare professionals and the general public to recognize the multitude of presentations of OCD. Access to therapy is critical in helping individuals develop healthier coping strategies and managing symptoms effectively. Understanding these varying symptoms allows individuals with OCD to feel less isolated, emphasizing that they are not alone and that there are effective resources available to help them on the path to recovery.
Myth 3: Medication is the only solution for OCD. While medication can be effective, it’s not the sole treatment option. Therapy plays an essential role in managing OCD symptoms. Cognitive-behavioral therapy (CBT), particularly exposure and response prevention (ERP), has been proven highly effective for reducing symptoms. This therapy teaches individuals to confront their fears gradually, aiding them in resisting compulsive behaviors. It’s vital not to dismiss therapy in favor of solely relying on medication. Many individuals benefit greatly from a combined approach, integrating both therapy and medication for a comprehensive treatment plan. The journey to recovery can be unique for everyone, and a well-rounded strategy helps create tailored solutions fitting each person’s needs. Understanding this balance empowers individuals to make informed decisions about their mental health care. Open conversations with health professionals can guide individuals to the most effective treatment path. They can address concerns, tailor interventions accordingly, and monitor progression over time. By recognizing the diversity in treatment options for OCD, we can foster an environment that encourages individuals to seek help without fear of stigma or judgment. Advocacy for comprehensive treatment models is vital in managing mental health.
Seeking Help for OCD
Fact: Early intervention is key. The sooner a person seeks help for OCD, the better their chances for recovery and intervention. This is particularly crucial since untreated OCD can lead to increased impairment and may exacerbate symptoms over time. Professionals recommend reaching out for help if obsessive thoughts or compulsive behaviors start interfering with daily life. Developing support systems, whether through family, friends, or support groups, can also provide relief and understanding. There are available resources such as hotlines, counselling, and online support communities that offer guidance. Engaging with others who understand the condition fosters a sense of belonging and support. Furthermore, mental health professionals equipped with the knowledge of OCD can design tailored interventions that address specific symptoms. Normalizing the process of seeking help can also motivate others to reach out when they begin noticing OCD traits within themselves or loved ones. It’s vital for society to create environments that encourage seeking assistance without shame. Through understanding and awareness, stigma diminishes, enabling individuals to address their struggles openly. Recognizing the importance of early intervention allows for greater success in managing OCD effectively.
In conclusion, understanding Obsessive-Compulsive Disorder is vital for reducing stigma and promoting effective treatment options. As we’ve explored, many myths surround OCD that can hinder individuals from seeking help or receiving appropriate support. By acknowledging the facts, we can improve awareness and compassion towards those affected. Acknowledging that OCD is a legitimate and complex mental health condition can foster empathy and encourage discussions about mental health. Each story is unique and deserves to be heard without judgment. As a community, we must advocate for better resources and continued education around OCD. Supporting one another while dismantling harmful myths creates a more inclusive and understanding environment. It is crucial to remember that recovery from OCD is possible with the right tools and support. Mental health struggles should not be stigmatized, and seeking help should be normalized. By educating ourselves and spreading awareness, we can contribute to a society where individuals feel empowered to share their experiences without fear. Together, we can create a culture of understanding that appreciates the complexity of OCD, emerging with solutions that prioritize mental health support for everyone.