The Impact of Non-Celiac Gluten Sensitivity on Sleep Quality
Non-Celiac Gluten Sensitivity (NCGS) is a condition that can profoundly influence various aspects of life, particularly sleep quality. While not as widely discussed as celiac disease, NCGS affects many individuals who experience gastrointestinal and extra-intestinal symptoms after consuming gluten. Sleep disturbances associated with NCGS may stem from different factors such as inflammation, gut dysbiosis, or immune responses. Furthermore, the emotional burden of managing dietary restrictions often amplifies the challenges faced by those with NCGS. Sleep is crucial for overall well-being and resilience, and disruptions can lead to significant fatigue and cognitive dysfunction. The relationship between gluten sensitivity and sleep is complex and multifaceted; it involves more than just dietary adjustments. Systematic research is essential to uncover the extent and nature of this relationship. Recognizing the impact of NCGS on sleep quality can help provide better support and management strategies for those affected. Additionally, educating healthcare professionals about NCGS may lead to improved diagnoses and treatments for patients struggling with related sleep issues.
Individuals with Non-Celiac Gluten Sensitivity often report a range of sleep problems, including insomnia, restless legs syndrome, and poor overall sleep quality. Ayurvedic practices and other holistic approaches suggest that diet plays a crucial role in sleep health. Gluten’s impact on gastrointestinal health directly correlates with sleep disturbances. For instance, inflammation from gluten intake may lead to disrupted neural pathways essential for sleep regulation. Furthermore, many individuals with NCGS experience anxiety or depression linked to dietary restrictions. These emotional states significantly contribute to reduced sleep quality. Poor sleep has a cyclic effect on emotional and mental well-being, encouraging a vicious cycle for those with NCGS. This complexity necessitates an integrative approach to treatment, considering both dietary and psychological factors. Potential interventions might include working with nutritionists who specialize in gluten-free diets, as well as therapists who can address emotional struggles. Additionally, mindfulness practices and sleep hygiene can play vital roles in overcoming sleep disturbances. Ultimately, addressing all contributing factors is essential to improving sleep quality for those affected by NCGS.
The Role of Inflammation
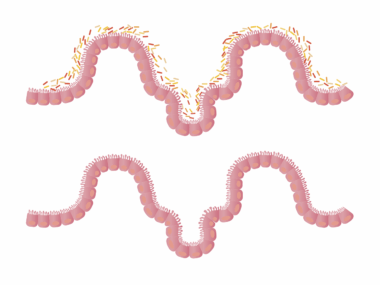
Inflammation is a common symptom experienced by individuals diagnosed with Non-Celiac Gluten Sensitivity. This inflammatory response can disrupt normal sleep patterns, leading to serious sleep quality issues. Research suggests that the body’s immune response to gluten can cause the release of pro-inflammatory cytokines, which directly affect the central nervous system. When inflammation persists, it can lead to physical discomfort and pain, both of which hinder the ability to fall and stay asleep. Inflammation’s effects on sleep include an increase in pain sensitivity and altered sleep architecture, diminishing the quality of restorative sleep. Understanding how gluten impacts inflammation can be a crucial step towards alleviating ailments associated with NCGS. Those experiencing symptoms may benefit from specific dietary interventions aimed at reducing inflammation, such as incorporating anti-inflammatory foods. Omega-3 fatty acids, antioxidants, and a diet rich in fruits and vegetables can all contribute to reducing systemic inflammation. Mindful eating, stress reduction strategies, and regular physical activity are also essential for managing inflammation. By addressing these elements, individuals with NCGS can significantly enhance their sleep quality.
A significant number of patients with Non-Celiac Gluten Sensitivity notice improvements in sleep quality after eliminating gluten from their diets. This dietary change not only relieves gastrointestinal distress but also helps mitigate the broader systemic symptoms associated with NCGS. Studies have found that adherence to a strict gluten-free diet may lead to improved mood, reduced fatigue, and better sleep. However, while dietary changes can have positive effects, they can also be a source of stress. The challenge of avoiding gluten can lead to increased anxiety, particularly in social situations where food choices may be limited. This emotional tension may, in turn, affect sleep negatively. To promote healthy sleep for individuals with NCGS, a holistic support system is vital. This includes nutritional education, psychological support, and connected community resources. Engaging in support groups can provide individuals with the emotional tools necessary to navigate their dietary restrictions. Moreover, exploring alternative therapies, like yoga or mindfulness meditation, can improve resilience against stress, thereby promoting better sleep. Continued research is essential to understand these dynamics more clearly.
The Psychological Component
The psychological impact of Non-Celiac Gluten Sensitivity cannot be understated, particularly as it relates to sleep quality. Anxiety, depression, and stress are prevalent among those managing NCGS, contributing significantly to sleep disturbances. The burden of potential food reactions may heighten the sense of uncertainty and fear, further complicating emotional and mental health. Chronic stress can inhibit the body’s ability to follow natural sleep cycles, leading to insomnia and fatigue during waking hours. To mitigate these psychological effects, creating a routine that prioritizes mental well-being may help. Incorporating regular exercise, practicing mindfulness or meditation, and maintaining a steady sleep schedule are vital elements in improving mental health and, by extension, sleep quality. Therapy, whether group or individual, can also provide valuable techniques for managing anxiety linked to dietary restrictions. Moreover, cognitive behavioral therapy (CBT) has shown promise in addressing sleep issues. By exploring gastrointestinal symptoms associated with NCGS and their emotional repercussions, individuals can learn to manage their anxieties more effectively. Ultimately, addressing the psychological dimension of NCGS is crucial for achieving better sleep outcomes.
The relationship between Non-Celiac Gluten Sensitivity and sleep quality underscores the importance of a holistic approach to treatment and management. Individuals affected by NCGS must pay attention to their dietary habits while also considering the psychological ramifications surrounding their condition. Regular consultations with healthcare providers, nutritionists, and mental health professionals are essential to provide a well-rounded support system. This coordinated approach can help individuals navigate the complexities of their condition more effectively, leading to improved sleep quality. Ongoing education about gluten sensitivity and its potential impact on various aspects of life is incredibly beneficial for both patients and caregivers. Accessibility to resources, research, and community support contributes to reducing the social stigma associated with gluten-related disorders. As more individuals recognize the intricate connection between diet, emotional health, and sleep, there is hope for future advancements in treatment options. Building a strong personal support network can also play a pivotal role in improving mental health and sleep outcomes. As the conversation around gluten sensitivities continues to grow, so will awareness and understanding, making it easier for sufferers to find relief.
Conclusion
The intersection of Non-Celiac Gluten Sensitivity and sleep quality highlights an essential area of concern for many individuals. Affected persons must proactively seek ways to improve their sleep and manage symptoms through diet, mindfulness, and therapy. Exploring various strategies to alleviate stress and emotional turmoil is equally important. Those suffering from NCGS should consider working closely with healthcare teams who understand the intricacies of this condition. Outside of strict dietary adjustments, exploring therapies and holistic methods will cultivate a comprehensive approach to enhancing well-being. While understanding NCGS is still evolving, increasing awareness can lead to improved quality of life for individuals. Learning about available resources and connecting with others experiencing similar challenges can provide essential support and validation. Practicing self-care is fundamental and engaging in open discussions about individual experiences will foster community and resilience. Research continues to shed light on gluten-related disorders, emphasizing the need for tailored dietary and psychological interventions. Ultimately, addressing both dietary and emotional health concerns will promote better sleep and overall wellness.
Overall, Non-Celiac Gluten Sensitivity presents a unique challenge that requires multifaceted strategies to manage effectively. Disruptions in sleep quality can severely impact daily life, yet understanding the holistic connection between diet, emotions, and sleep can provide a clearer path to relief. By focusing on both dietary changes and emotional support structures, individuals may find themselves better equipped to handle the effects of gluten sensitivity. Ongoing learning and adaptation are necessary for living well with NCGS and ensuring that it does not diminish one’s quality of life. Encouraging research into the broader implications of NCGS will pave the way for innovative approaches in treatment and lifestyle adaptation. As knowledge continues to grow, it offers hope and guidance for those navigating their journey with gluten-related sensitivities. Each person’s experience is unique, yet the common thread of managing sleep quality binds them together. Through collaboration between researchers, healthcare professionals, and patients, effective strategies can be developed to mitigate adverse effects. As we further investigate NCGS, we can anticipate a more profound understanding of its role on sleep and healthier living for all affected.