How Stress Management Can Improve Diabetic Neuropathy Outcomes
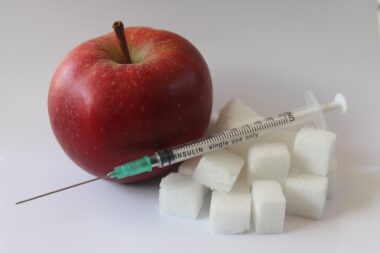
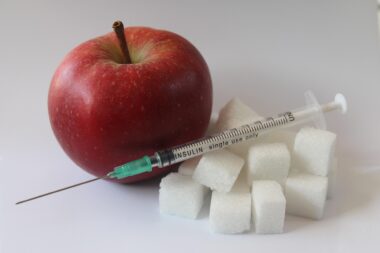
Diabetic neuropathy is a common complication resulting from diabetes that affects the nervous system. Individuals experiencing diabetic neuropathy often suffer from debilitating symptoms, including pain, numbness, and tingling in the extremities. These symptoms can significantly impact daily living and overall quality of life. Effective management of stress plays a crucial role in mitigating symptoms associated with diabetic neuropathy. Stress can exacerbate pain and worsen overall health, leading to further complications. Reducing stress through various techniques can help in alleviating some of the discomfort experienced. Exploring methods such as mindfulness, meditation, and physical exercise may offer additional relief. Notably, incorporating relaxation strategies into daily routines can create a more balanced emotional state. Furthermore, managing stress can result in better glycemic control, which is vital in diabetic patients. When blood glucose levels are stabilized, the progression of neuropathy may be slowed or even reversed in some individuals. It’s essential to engage in supportive communities, as conversation and sharing experiences can significantly reduce feelings of isolation and stress.
Another crucial aspect of managing stress linked to diabetic neuropathy is creating a structured daily routine. A consistent schedule can alleviate anxiety regarding unpredictable spikes in blood sugar levels, thereby enhancing emotional stability. Eating regular meals and managing medication timing effectively can go hand-in-hand with routine. Developing healthy eating habits is essential; a balanced diet is known to ease stress. Foods rich in omega-3 fatty acids, antioxidants, and certain vitamins may reduce inflammation. Increased inflammation can often worsen neuropathic symptoms, leading to heightened pain and distress. Additionally, keeping a food journal can help identify any dietary triggers that exacerbate symptoms. Gentle physical activities such as yoga or tai chi can be integrated into daily practice to improve both mental and physical health. These activities are proven beneficial for enhancing peripheral circulation, which can positively impact diabetic neuropathy. Furthermore, always consulting healthcare professionals for tailored advice and treatments remains critical. Addressing stress holistically, in conjunction with medical care, forms a more comprehensive approach to better outcomes in diabetic neuropathy management.
Understanding the importance of sleep cannot be overstated when it comes to stress management for individuals with diabetic neuropathy. Poor sleep quality can lead to increased pain perception and a lower tolerance for stress. Establishing a calming bedtime routine can significantly enhance sleep quality. Steps like minimizing screen time and creating a sleep-conducive environment can promote deeper rest. Additionally, relaxation techniques, such as reading or listening to calming music before sleep, can be helpful. Evidence suggests that adequate sleep improves cognitive function and emotional well-being, thus influencing how one perceives and reacts to pain. Enhanced cognitive function also aids in better decision-making related to health management. Moreover, establishing a sleep schedule that includes going to bed and waking up at the same time daily can enhance overall sleep patterns. This small change can produce substantial effects on both physical and emotional health, leading to better diabetes management outcomes. Encouraging supportive relationships can also provide emotional comforts, effecting improvements in pain management. Thus, prioritizing sleep acts as a critical component in managing stress and diabetic neuropathy.
Support Networks and Their Role
Creating social support networks is invaluable for those coping with diabetic neuropathy and associated stress. Surrounding oneself with understanding individuals can foster an environment of compassion and keep a person motivated. Groups, whether online or in-person, such as diabetic support groups, offer a safe space for individuals to share experiences and emotional struggles. These social interactions can significantly enhance feelings of belonging, which may help individuals maintain perspective on their challenges. Furthermore, support groups can provide not only emotional support but also practical advice on managing diabetic neuropathy. Cognitive Behavioral Therapy (CBT) is another fantastic resource for individuals struggling with pain and discomfort. CBT, often facilitated within support settings, can provide coping strategies for managing stress effectively. Families also play a critical role in providing emotional support. Encouraging honest conversations about distress can facilitate a holistic approach to treatment. Involving family members in care planning can enhance accountability and be beneficial for both emotional and physical well-being. Support networks increase resilience and efficacy in managing the complexities of diabetic neuropathy.
Another significant aspect of stress management involves setting achievable goals tailored to individual circumstances. When dealing with diabetic neuropathy, focusing on realistic targets can bolster confidence and reduce overwhelming feelings. Goals can relate to dietary modifications, exercise routines, or overall wellness habits. Gradual progress towards these goals creates a sense of accomplishment, inherently reducing stress levels. Additionally, writing down motivated goals can serve as a powerful reminder, encouraging persistence. It’s essential to celebrate even minor successes, as they contribute to long-term behavioral change. Positive reinforcement can effectively foster a hopeful mindset, most essential for those managing chronic conditions. Balancing ambition with patience is crucial; progress takes time, and setbacks may occur along the journey. Maintaining an optimistic mentality not only alleviates stress but also significantly impacts overall health outcomes associated with diabetic neuropathy. Engaging in reflective practices can also enhance emotional maturity, allowing individuals to process experiences constructively. Regularly assessing one’s emotional state can identify potential stressors and inform effective coping strategies.
Incorporating professional assistance for stress management is another benefit every diabetic should consider. By consulting healthcare professionals like therapists or psychologists, individuals can access various tools designed to help with stress reduction. Therapists trained in pain management specifically can demonstrate methods tailored to chronic conditions like diabetic neuropathy. Having a qualified expert guide you helps ensure effective strategies are utilized; this can be especially comforting during moments of crisis. Many healthcare providers offer frameworks or guidance that propels better coping mechanisms to handle stress. Implementing techniques like mindfulness meditation or biofeedback can greatly enhance relaxation and emotional regulation. Not only can professionals provide emotional support, but they can also monitor psychological well-being over time. If needed, therapy could also aid in addressing any underlying mental health disorders contributing to stress, such as anxiety or depression. While independent stress management techniques are helpful, the combined benefits of professional interventions may yield enhanced coping capabilities. Thus, seeking professional help is a solid step towards managing both stress and diabetic neuropathy effectively.
Conclusion
The connection between stress management and diabetic neuropathy outcomes is vital for effective treatment. Individuals with diabetic neuropathy can significantly enhance their quality of life through proactive stress reduction strategies. Understanding that ongoing management can pave the way towards meaningful improvements ensures personalized care is at the forefront of treatment. By engaging in supportive networks, establishing structured routines, and employing practical stress management techniques, numerous emotional and physical benefits can be experienced. Regular evaluations with healthcare professionals can tailor and refine approaches to stress, enhancing efficacy over time. Importantly, self-care should remain a priority, factoring in nutrition, sleep, and emotional well-being. Each component collectively adds to a holistic approach addressing the multifaceted nature of diabetic neuropathy. Encouraging emotional intelligence and resilience in the face of adversity can lead to improved health outcomes. Individuals facing diabetic neuropathy may realize that managing stress serves not only to reduce symptoms but also to regain control over their lives. Adapting strategies and continually learning about individual needs empowers patients in improving their lives significantly despite challenges.
This is another paragraph with exactly 190 words…