The Role of Medication in Diabetes Control
Managing diabetes effectively is crucial for a person’s health, as it can lead to serious complications when poorly controlled. One key aspect of diabetes management is the use of medications, which are prescribed to help control blood sugar levels. Medications can take several forms, including oral medications, insulin, and other injectable treatments. Each medication works differently, targeting blood sugar levels through various mechanisms. For example, some medications increase insulin sensitivity, while others stimulate insulin production. It’s essential for individuals with diabetes to work closely with healthcare professionals to determine the best medication plan tailored to their specific needs. In addition to medications, lifestyle choices such as diet and exercise also play a significant role in diabetes management. Healthcare providers may suggest monitoring blood sugar levels regularly to assess how well the medications are working. Patient education is vital to ensure that individuals understand their medications, potential side effects, and the importance of adhering to prescribed regimens. Combining medication with a healthy lifestyle promotes better outcomes and improves the overall quality of life for patients with diabetes. A well-rounded diabetes management plan ultimately fosters better health and well-being.
Types of Diabetes Medications
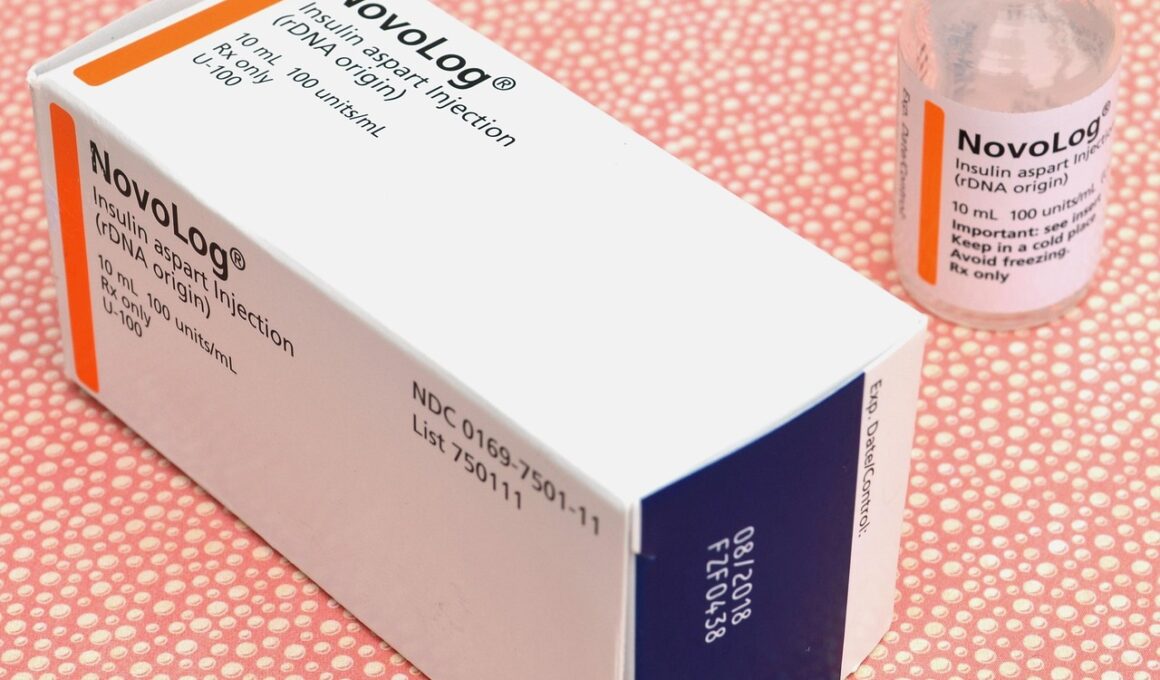
There are various types of medications available for managing diabetes, each targeting specific aspects of blood sugar control. Oral medications are commonly prescribed for type 2 diabetes and include classes like biguanides, sulfonylureas, and DPP-4 inhibitors. Biguanides, like Metformin, work by reducing insulin resistance and lowering liver glucose production. Sulfonylureas stimulate the pancreas to release more insulin, while DPP-4 inhibitors increase incretin levels, which help regulate insulin and blood sugar. Additionally, thiazolidinediones improve insulin sensitivity but may carry certain risks, necessitating discussion with healthcare providers. For individuals with type 1 diabetes, insulin therapy is essential, as their bodies do not produce insulin. Insulin can be delivered through various methods, such as syringes, pens, or pumps. Moreover, newer classes of medications, like GLP-1 receptor agonists and SGLT2 inhibitors, have emerged, offering innovative ways to control blood sugar levels. The choice of medication can depend on several factors, including individual preferences, lifestyle, medical history, and potential side effects. Regular communication with a healthcare team is vital to optimize diabetes management strategies across diverse patient populations.
The Importance of Blood Sugar Monitoring
Regular blood sugar monitoring is crucial for individuals with diabetes to ensure adequate control over their condition. By tracking blood glucose levels, patients can understand how different foods, medications, and physical activities impact their diabetes management. Tools such as glucometers and continuous glucose monitors (CGMs) make it easier to obtain real-time data regarding blood sugar levels. Blood sugar testing frequency may differ based on individual needs and treatment plans. For instance, those on insulin therapy may need to check their levels multiple times daily, whereas those utilizing oral medications may need to monitor less frequently. Understanding the significance of blood sugar levels is essential for making informed decisions about diet and medication adjustments. Sudden spikes or drops in glucose can lead to serious health complications, including hypoglycemia or long-term organ damage. Education plays a pivotal role in helping patients recognize the symptoms of both high and low blood sugar. This knowledge empowers individuals to respond proactively, avoiding severe consequences. Furthermore, consulting healthcare providers helps to refine testing regimens and interpret results, ultimately fostering better health outcomes and a more robust diabetes self-management strategy for those affected.
Medication adherence is essential for managing diabetes effectively and achieving optimal health outcomes. When patients follow their prescribed treatment regimen diligently, blood sugar levels stabilize, reducing the risk of complications. Medication non-adherence can stem from various factors, such as forgetfulness, side effects, or a lack of understanding about the importance of the treatment. Practical strategies can help enhance adherence, including setting reminders, using pill organizers, and scheduling regular follow-ups with healthcare providers. Building a strong support system encompassing family, friends, and diabetes educators can also motivate patients to remain compliant with their medication regimens. Moreover, patients should maintain open communication with their healthcare team regarding any difficulties they may encounter. It is crucial for healthcare providers to address patient concerns, adjust treatment plans, and offer additional resources when needed. Personalized education will ensure that individuals understand how their medications help control their condition and the consequences of not adhering to the prescribed regimen. Fostering a patient-centered approach in diabetes care encourages active participation of individuals in their treatment processes, ultimately resulting in better health management and improved quality of life for those living with this chronic condition.
The Role of Lifestyle in Diabetes Management
While medications are vital for controlling diabetes, lifestyle factors also play an equally significant role in achieving optimal health. A well-balanced diet tailored to individual needs can help regulate blood sugar levels effectively. Consuming a variety of whole foods, such as fruits, vegetables, whole grains, lean proteins, and healthy fats, ensures that patients receive the necessary nutrients. Understanding carbohydrate counting and portion control can also positively impact blood sugar management. Physical activity presents another critical element of a healthy lifestyle; it aids in weight management while improving insulin sensitivity. Engaging in regular exercise, such as walking, swimming, or strength training, helps lower blood sugar levels and can reduce the need for medication in some cases. Stress management is equally essential, as high-stress levels can negatively impact glucose levels. Techniques such as mindfulness, meditation, and relaxation exercises can help mitigate stress and improve overall well-being. A holistic approach to diabetes management encompasses medication adherence, a balanced diet, regular exercise, and stress reduction, fostering a healthier life for those living with diabetes. Collaborating with healthcare providers can ensure that each patient develops a customized lifestyle plan to optimize their diabetes management.
Potential Side Effects of Diabetes Medications
Like any medication, diabetes treatments can carry potential side effects that patients should be aware of to make informed decisions. Common side effects from oral medications may include gastrointestinal issues, such as nausea and diarrhea, particularly with Metformin. For insulins, patients may face the risk of hypoglycemia, which occurs when blood sugar levels drop too low. Other side effects can include weight gain, especially with certain insulin secretagogues and thiazolidinediones. It’s crucial for individuals to monitor their responses to these medications closely and discuss any experiences with their healthcare providers. Understanding the risks associated with each medication allows patients to prioritize their well-being effectively. In some cases, switching or adjusting medications may be necessary to minimize side effects. Healthcare providers may also suggest combining medications with lifestyle changes to mitigate potential adverse effects. Open dialogue facilitates better medication management and ensures that individuals can continue their treatment without experiencing undue complications. Ultimately, recognizing possible side effects helps empower diabetes patients, providing them with the tools necessary for proactive management and improved long-term health outcomes.
Conclusion and Future Directions
As the understanding of diabetes evolves, the role of medication continues to be a fundamental aspect of effective management. Research advances are leading to the development of innovative diabetes medications continuously designed to enhance outcomes for patients. New drug classes, such as SGLT2 inhibitors and GLP-1 receptor agonists, demonstrate potential benefits beyond blood sugar control, including cardiovascular and renal protection. These advancements reflect the trend towards personalized medicine, allowing clinicians to tailor treatments based on individual patient profiles and responses. Additionally, emerging technologies, including digital health solutions and telehealth, are becoming increasingly integrated into diabetes management. Remote monitoring tools can enhance patient engagement in their care, enabling real-time adjustments, feedback, and support. Furthermore, ongoing education for both patients and healthcare professionals is essential in optimizing strategies for diabetes management. By focusing on individualized treatment plans incorporating medications, lifestyle modifications, and patient education, people living with diabetes can achieve better health outcomes. As we look to the future, collaboration between patients, caregivers, and healthcare providers will play a critical role in shaping the diabetes care landscape, ensuring optimal results for individuals around the globe.
Maintaining a healthy breakfast routine can positively influence blood sugar levels throughout the day. Incorporating fiber-rich foods into your breakfast, such as oats or whole-grain toast, can help maintain stable glucose levels. A balanced breakfast can also curb cravings and prevent overeating later in the day. Additionally, pairing carbohydrates with protein or healthy fats can further support blood sugar management. Healthy protein options for breakfast include eggs, Greek yogurt, or nut butter. If you’re interested in learning more about diabetes-friendly breakfast ideas, consulting with a registered dietitian can provide tailored insights and recommendations. Small, mindful changes to your breakfast can lead to significant improvements in glucose control over time. Knowing how to make informed choices empowers you to create a meal plan that works for your lifestyle and diabetes management goals. As you implement these strategies, be sure to track your blood sugar levels to determine how different foods affect your body. Remember, consistency is key. Developing a routine will enhance your overall diabetes management, leading to better health outcomes and improved quality of life.