Therapeutic Ultrasound in Muscle Strain Rehabilitation
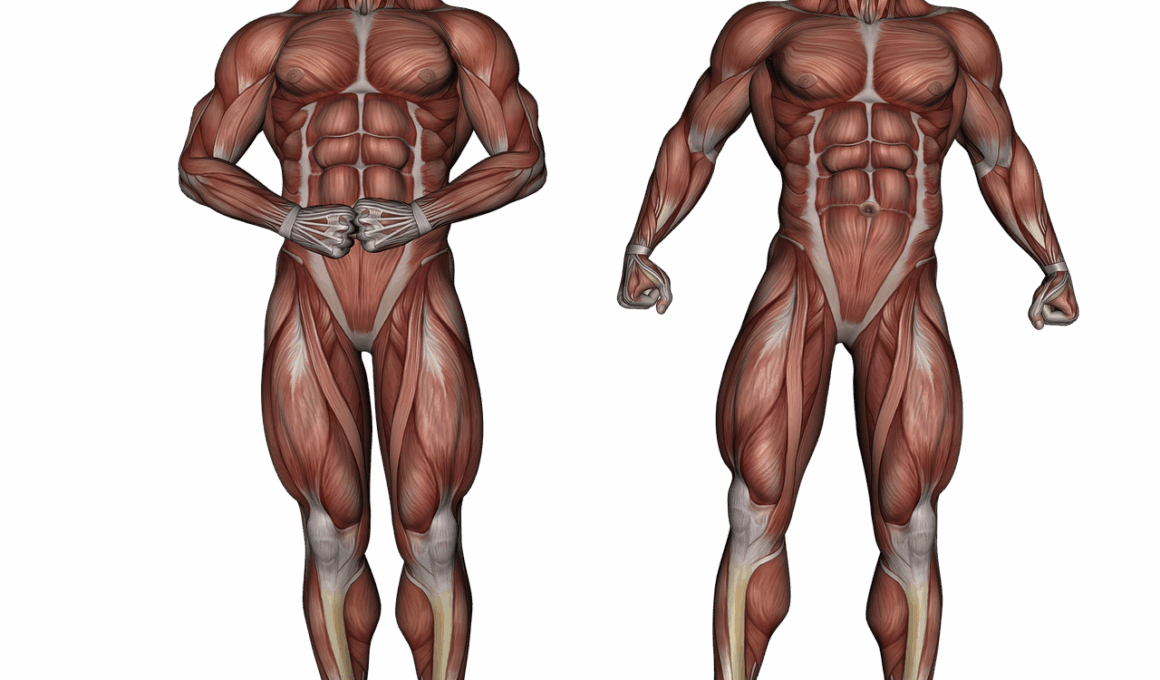
Therapeutic ultrasound is a widely used modality in the rehabilitation of muscle strains. This technique involves the application of sound waves to induce various biological effects. The primary advantages of ultrasound therapy include promoting tissue healing, reducing inflammation, and alleviating pain. Sound waves penetrate deep into the tissues, which can improve blood flow and cell metabolism. As such, therapeutic ultrasound has become a cornerstone in physical therapy programs. The depth of penetration makes it particularly effective for treating deeper muscle strains. Additionally, it can be integrated into various treatment protocols, combining ultrasound with exercises for optimal recovery. Clinicians often tailor treatment plans to individual needs, ensuring maximum efficacy. It is crucial to administer therapeutic ultrasound safely and effectively to avoid potential side effects. The use of coupling agents, like gels, enhances the transmission of sound waves. Clinicians must possess the necessary skills to apply this therapy correctly. Regular assessments during treatment can help gauge the patient’s progress and adjust modalities accordingly. Thus, therapeutic ultrasound serves as a key technique for physical therapists in managing muscle strains.
Muscle strains can significantly impact an individual’s daily activities and athletic performance. Thus, understanding the components of therapeutic ultrasound is essential for optimal results in rehabilitation. Therapeutic ultrasound uses high-frequency sound waves that create thermal and non-thermal effects on body tissues. This therapy’s thermal effects involve increasing tissue temperature, which enhances collagen tissue extensibility and can improve the healing process. In contrast, the non-thermal effects stimulate cellular processes, facilitating tissue repair at the cellular level. There are distinct mechanisms involved, including cavitation, which causes micro-bubbles in the tissues to form and collapse, promoting cellular responses. Unlike other modalities, ultrasound can target specific areas while minimizing the effects on surrounding tissues. The treatment can last between five to 15 minutes per session depending on the extent of the injury. Protocols often revolve around patient tolerance and injury severity. Regular treatments usually occur multiple times a week to ensure a consistent therapeutic effect. As rehabilitation progresses, modalities may be altered to incorporate functional movements. Educating patients about ultrasound therapy’s goals can enhance adherence and positive outcomes.
Indications and Contraindications
Identifying proper indications and contraindications for therapeutic ultrasound is crucial for any physical therapist. Common indications include muscle strains, tendon injuries, and ligament sprains. These conditions often benefit from ultrasound’s ability to speed up the healing process significantly. Furthermore, ultrasound therapy can help in managing acute injuries, where inflammation and swelling are present. However, it is paramount to avoid using ultrasound on individuals with certain contraindications. These include pregnancy, over malignant tumors, or infections in the targeted area. Additionally, recent fractures and bleeding disorders can also prohibit the use of this therapy. Precaution should be taken when treating patients with sensory or circulatory deficits. Thorough assessments at initial evaluations are essential. Therapists should gather comprehensive medical histories to ensure the safety and well-being of patients. Informed consent prior to treatment sessions also plays an essential role in establishing a trusting therapist-patient relationship. By clarifying any uncertainties concerning therapeutic ultrasound, therapists can empower patients. Awareness of the treatment’s benefits and risks fosters a collaborative atmosphere and improves patient engagement during recovery.
The application of therapeutic ultrasound can vary depending on the phase of injury recovery. Early rehabilitation phases prioritize reducing inflammation and pain, while later phases focus on tissue repair and enhancing mobility. In the initial stages, physical therapists might apply ultrasound to decrease swelling effectively. This action promotes better circulation and prepares the body for subsequent rehabilitation exercises. Over time, as pain subsides and healing progresses, the focus shifts to improving range of motion and strength through rehabilitative exercises. Incorporating therapeutic ultrasound into a comprehensive rehabilitation program can provide more effective outcomes. Furthermore, combining ultrasound with electrical stimulation can enhance muscle activation. This multimodal approach addresses various components of recovery. For instance, patients may benefit from both therapies simultaneously, resulting in more comprehensive healing. Therapeutic ultrasound also opens opportunities for education regarding self-management and home exercise programs. Knowledge gained through therapy can empower patients to engage fully in their recovery process actively. As patients progress, the therapist may increase the intensity and complexity of exercises. Adaptable protocols based on the patient’s individual progress ensure that treatment remains effective and timely.
Research and Evidence
Studies surrounding therapeutic ultrasound have reinforced its significance in muscle strain rehabilitation. Evidence increasingly supports the modality’s efficacy in promoting faster healing rates. Clinical trials have demonstrated that patients receiving ultrasound therapy recover sooner than those undergoing traditional treatments. Research suggests that the combination of thermal and non-thermal effects can enhance overall rehabilitation outcomes. Furthermore, randomized control trials have noted that ultrasound therapy has a significant influence on reducing pain perception among patients. In chronic cases, ultrasound treatments also exhibit a decrease in muscle tightness and stiffness. As research continues to evolve, identifying the specific parameters that maximize therapeutic effects becomes crucial. Parameters include frequency, intensity, and duration, which can be adjusted depending on each patient’s response to treatment. Consequently, ongoing education for physical therapists ensures that they remain current with the latest developments in ultrasound therapy. This knowledge empowers them to modify treatment effectively. Patients, too, benefit from knowing that contemporary practices reflect the latest evidence in therapy. Awareness of advancements leads to increased trust between the patient and therapist, contributing to a successful rehabilitation experience.
Challenges still exist in the broader acceptance and implementation of ultrasound therapy in clinical settings. Many practitioners remain hesitant due to misconceptions about its efficacy. Additionally, limited systematic reviews on therapeutic ultrasound could affect widespread adoption. Moreover, variations in clinical practice guidelines can lead to inconsistent applications of ultrasound therapy. Addressing these challenges necessitates continued dialogue between professionals in the physical therapy community. Conferences, workshops, and collaborative studies can pave the way for exploring best practices. Encouraging standardization in treatment protocols may help overcome fragmentation in practitioners’ approaches to ultrasound therapy. As consensus builds around treatment guidelines, more patients may benefit from this modality. Furthermore, newly emerging technologies can support the implementation of therapeutic ultrasound in everyday practice. Devices that simplify the application process provide confidence to physical therapists. This step is essential in ensuring that patients receive optimal care. Exploring the integration of ultrasound therapy with other rehabilitation techniques shows promise for improved outcomes. Investigating the synergistic effects of combining modalities could lead to enhanced recovery pathways for patients. Ultimately, developing a unified approach offers the potential for more research and innovation in the field.
Conclusion
In conclusion, therapeutic ultrasound plays a vital role in the rehabilitation of muscle strains. Its diversity in benefits, including pain reduction and tissue healing, makes it indispensable in the physical therapy toolbox. As understanding of this modality continues to grow, practices will likely become more standardized and evidence-based. Clinicians must remain attuned to advancements and effective protocols for implementing ultrasound therapy. A comprehensive approach that integrates ultrasound with other rehabilitation techniques can optimize patient outcomes. Furthermore, patient engagement and education are fundamental to successful recovery journeys. As therapists equip patients with knowledge and self-management skills, adherence to treatment plans improves. Therapeutic ultrasound’s adaptability in various stages of rehabilitation contributes to its effectiveness. Ongoing research is critical to ensuring that ultrasound practices evolve in alignment with the latest scientific findings. By fostering collaboration and communication among healthcare professionals, a more significant understanding of ultrasound therapy can emerge. As physical therapists champion patient-centered care, the commitment to enhancing recovery experiences with therapeutic ultrasound will endure. Emphasizing collaboration between patients and therapists will ultimately serve to drive successful rehabilitation outcomes.